How Do Breast Cancer Screening Rates Compare Among Different Groups in the U.S.?
Read our blog, The Racial Injustice of Breast Cancer.
Screening mammography is important for all women, regardless of their race/ethnicity and their risk of breast cancer. Along with follow-up tests, and treatment if diagnosed, mammography can reduce the chance of dying from breast cancer.
Some women are less likely than others to get screening mammograms. There are many reasons for inequities in breast cancer screening in the U.S. Some are described here.
Learn about Susan G. Komen®’s work in advancing health equity.
Health insurance
A main reason behind differences in screening mammography rates in the U.S. is health insurance.
Women without health insurance are much less likely than women with health insurance to get screening mammograms.
In 2021 (most recent data available), among women ages 50-74 [162]:
- 42% of those without health insurance had a screening mammogram in the past 2 years
- 71% of those with Medicaid or other public health insurance had a screening mammogram in the past 2 years
- 80% of those with private health insurance had a screening mammogram in the past 2 years
In 2021 (most recent data available), among women ages 65 and older [162]:
- 75% of those on Medicare had a screening mammogram in the past 2 years
Although a lack of health insurance is a main reason for breast cancer screening inequities in the U.S., other factors play a role. As shown above, even among women ages 50-74 who had insurance, only 71% to 80% had a recent screening mammogram [162].
Since September 2010, the Affordable Care Act has required all new health insurance plans to cover screening mammograms with no co-payment [19]. Health plans must cover screening mammography at least every 2 years for women 50 and older, and as recommended by a health care provider for women 40-49 [19].
Learn more about Medicare, Medicaid and insurance company coverage of mammograms.
Find resources for low-cost or free mammograms.
Learn about health insurance.
Other barriers to breast cancer screening
Other barriers to mammography screening may include [65,115-120,162]:
- Low income or worry about cost
- Lack of access to care (such as lack of transportation to a mammography center)
- Lack of a usual health care provider
- Lack of a recommendation from a health care provider to get mammography screening
- Low education level
- Lack of knowledge of breast cancer risks and screening methods
- Lack of child or elder care
- Lack of sick leave or unable to miss work
- Fear of bad news or pain from the mammogram
- More recent migration to the U.S. (born outside the U.S. and living in the U.S. for less than 10 years)
- Cultural and language differences
These may explain some of the differences in screening mammography rates among certain populations of women, such as women from different racial and ethnic groups, as well as those who live in different areas of the country.
For example, women who live in rural areas, who may have limited access to health care, are less likely to get screening mammograms than women who live in urban areas [121].
Race and ethnicity
Screening mammography rates in the U.S. vary by race and ethnicity (see Figure 3.6 below).
Figure 3.6
|
|
Percentage of women ages 50-74 who had a screening mammogram in the past 2 years in 2021 (most recent data available) |
|
Black |
82% |
|
White |
76% |
|
Hispanic |
74% |
|
Asian |
67% |
|
American Indian and Alaska Native |
59% |
|
Adapted from American Cancer Society materials [162]. |
|
Black women in the U.S.
In 2021 (most recent data available), Black women had higher rates of screening mammography than other women [162].
Overall, the breast cancer incidence rate (rate of new cases) is lower among Black women than among white women [157].
However, the breast cancer mortality rate is higher in Black women (see Figure 3.7 below) [158].
For example, the breast cancer mortality rate from 2016 to 2020 (most recent data available) was about 39% higher for Black women than white women [158].
Figure 3.7
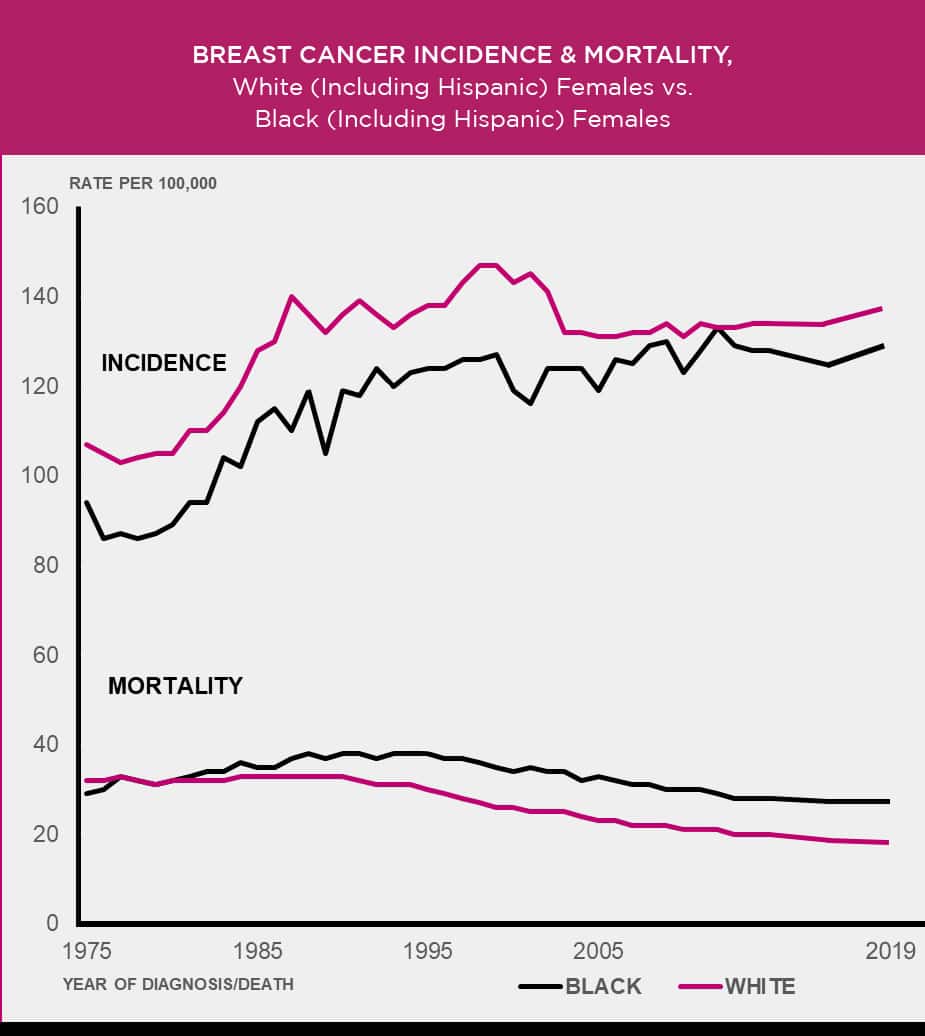
Age-adjusted to the 2000 U.S. standard population.
Source: 1975-2020 SEER data, 2023 [159-160]
Access to follow-up care for Black women
Access to follow-up care after an abnormal mammogram may explain part of the survival gap between Black women and white women.
Some findings have shown Black and African American women may have more delays in follow-up after an abnormal mammogram than white women [128-130].
Delays in follow-up may play a role in the lower survival rates among Black and African American women [131].
Other factors related to lower breast cancer survival among Black women
Even after accounting for differences in income and access to care, Black and African American women in the U.S. are diagnosed with more advanced breast cancers and have worse survival than white women [131-134,165].
Learn more about factors that may impact breast cancer risk and survival among Black women.
Learn about Susan G. Komen®’s work in advancing health equity.
Age at diagnosis for Black women
Black women in the U.S. who develop breast cancer tend to be diagnosed at a younger age than white women [167].
From 2016 to 2020, the median age at diagnosis for Black women was 60, compared to 64 for white women [167].
The median is the middle value of a group of numbers, so about half of Black women were diagnosed with breast cancer before age 60 and about half were diagnosed after age 60. Among white women, about half were diagnosed with breast cancer before age 64 and about half were diagnosed after age 64.
Hispanic/Latina women in the U.S.
In 2021 (most recent data available), Hispanic women had similar rates of screening mammography as white women, but lower rates of screening mammography compared to Black women (see Figure 3.6) [162].
However, some findings show Hispanic women may have a higher number of barriers to getting screening mammograms than women of other ethnicities [116,120].
Breast cancer screening among Hispanic/Latina women by group
Mammography screening among Hispanic/Latina women varies by group. For example, women of Central/South American origin have higher screening mammography rates than Mexican American women [136].
Compared to Hispanic women who have lived in the U.S. for a short period of time, those who have lived in the U.S. for a long period of time may be more likely to get mammograms [136].
The importance of mammography for Hispanic/Latina women
Hispanic women have lower rates of breast cancer and breast cancer mortality compared to non-Hispanic Black women and non-Hispanic white women [157-158].
However, breast cancer is still the most common cancer (and the leading cause of cancer death) among Hispanic women [166]. So, screening mammography is just as important for Hispanic/Latina women as it is for Black women and white women.
Hispanic women tend to be diagnosed with more advanced breast cancers than white women [136]. This may be due to more delays in follow-up care after an abnormal mammogram [136].
Asian American, Native Hawaiian and Pacific Islander women in the U.S.
In 2021 (most recent data available), Asian American women in the U.S. had lower rates of screening mammography compared to Black women, white women and Hispanic women [162].
However, compared to white women, Asian women in the U.S. have more delays in follow-up care after an abnormal mammogram [141].
Non-Hispanic Asian and Pacific Islander women tend to have lower rates of breast cancer and breast cancer mortality (death) than non-Hispanic Black women and non-Hispanic white women [157-158].
However, breast cancer is the second leading cause of cancer death in Asian and Pacific Islander women (lung cancer is the major cause of cancer death) [166]. So, screening mammography is just as important as it is for Black women and white women.
Native American and Alaska Native women
In 2021 (most recent data available, though data were limited), American Indian women and Alaska Native women had lower rates of breast cancer screening compared to other women [162].
Among women ages 50-74, 59% of American Indian and Alaska Native women had a mammogram in the past 2 years compared to 82% of Black women and 76% of white women (see Figure 3.6) [162].
One reason for these differences in screening rates may be access to care. American Indian and Alaska Native women tend to live in areas that require traveling a long distance to get health care, including screening mammography [137].
Breast cancer screening among American Indian and Alaska Native women by group
Screening mammography rates among American Indian and Alaska Native women vary depending on where women live [1]. Women who live in the Southern Plains and Alaska have higher rates of screening mammography than women who live in the Pacific Coast region [1].
The importance of mammography for American Indian and Alaska Native women
Breast cancer is the most common cancer among American Indian and Alaska Native women [166].
Non-Hispanic American Indian and Alaska Native women tend to have lower rates of breast cancer and breast cancer mortality than non-Hispanic Black women or non-Hispanic white women [157-158]. However, non-Hispanic American Indian and Alaska Native women are less likely than non-Hispanic white women to be diagnosed with early-stage breast cancer that has not spread to the lymph nodes [138].
Breast cancer rates vary according to where American Indian and Alaska Native women live.
American Indian and Alaska Native women who live in the Southern Plains, the Northern Plains and Alaska have the highest rates of breast cancer incidence, higher than incidence rates among white women in these areas [1,139-140]. Those who live in the Southwest and the East have lower rates [1,139-140].
Gay, lesbian and bisexual women, transgender people and nonbinary people
Listen to our Real Pink podcast, Breast Health in the LGBTQ+ Community.
Screening mammography rates among lesbians and bisexual women are similar to screening mammography rates among heterosexual women [162,165].
In 2021 (most recent data available) [162]:
- 78% of gay and lesbian women ages 50-74 had a mammogram in the past 2 years
- 76% of straight women ages 50-74 had a mammogram in the past 2 years
Data on screening mammography in transgender people and nonbinary people are limited.
Some lesbians and bisexual women may not get regular mammograms. This may be due to [144-145,165]:
- Lack of health insurance
- Perceived low risk of breast cancer
- Past discrimination or insensitivity from health care providers
- Low level of trust of health care providers
- Having trouble finding a health care provider
One step you can take is to find a health care provider who is sensitive to your needs. Getting a referral from a trusted friend may help. The National LGBT Cancer Network has a directory of LGBT-welcoming cancer screening centers that may be helpful.
Regular visits to a health care provider offer the chance to discuss your risk of breast cancer and get breast cancer screening and other needed health care.
Learn about breast cancer screening for transgender people.
Women with physical disabilities
Women with physical disabilities tend to get mammograms less often than women without such limitations [146-147]. One reason is lack of access to mammography centers that meet their needs [147-149].
Many mammography centers (especially mobile ones) simply aren’t designed for women who have trouble getting around.
Having a good experience increases the chances women with disabilities will return for routine mammograms [150].
If you have concerns about access, call the mammography centers in your area until you find one that meets your needs. Partnering with your health care provider in your search may help.
If access to mammography for women with disabilities is limited in your area, let your local medical centers know. This may help increase access for you and other women.
The CDC has a tip sheet for breast cancer screening for women with disabilities.
Getting involved
Women with disabilities know best how to improve mammography centers, medical equipment and patient-doctor relations.
Let your voice be heard. If access to health care for people with disabilities isn’t as good as it could be in your area, let your local medical centers, health insurance companies and elected officials know.
About 36 million women in the U.S. have a physical disability [151], making a powerful group to lobby for change.
|
What is Susan G. Komen® doing? |
|
Komen and the American Association on Health and Disability (AAHD) worked together to address and remove barriers to breast cancer screening and treatment for women with disabilities. Komen and AAHD launched Project Accessibility USA to improve care for women with disabilities and ensure access to high-quality breast cancer care for all. |
Removing barriers to screening
Many barriers may make it hard for some women to get breast cancer screening and follow-up on abnormal mammograms.
Increasing access, awareness and sensitivity may help remove some barriers (especially for women with low income who don’t have health insurance). This includes [65,120,152,162]:
- Improving access to mammography and primary care
- Removing financial barriers
- Removing language barriers
- Community education (such as health campaigns that address negative beliefs and feelings about mammography)
- Making sure health care providers are sensitive to the needs of women from different communities and cultures. When a provider doesn’t recommend a mammogram, some women don’t feel they need one.
The Affordable Care Act
Since September 2010, the Affordable Care Act has required all new health insurance plans to cover screening mammograms with no co-payment [19]. Health plans must cover mammography at least every 2 years for women 50 and older, and as recommended by a health care provider for women 40-49 [19].
Since the Affordable Care Act became law, the gaps in screening mammography between women with high-income and low-income levels have declined [153]. Gaps in screening mammography rates between women with high and low education levels also have declined [153].
Find resources for low-cost or free mammograms.
Talk with your health care provider about breast cancer screening
- If you’re at higher risk of breast cancer, talk with your health care provider about when to start breast cancer screening. You may need to be screened earlier and more often than other women. You may also benefit from other imaging, such as breast MRI.
- If you’re 40 or older (and at average risk of breast cancer), talk with your health care provider about breast cancer screening. Discuss when and how often you should get a mammogram.
Komen believes all women should have access to regular screening mammograms when they and their health care providers decide it’s best based on their risk of breast cancer.
Learn more about talking with your health care provider.
Get follow-up tests without delay
If your mammogram shows something abnormal, you’ll need follow-up tests to check whether or not the finding is breast cancer. A patient navigator at your medical center may help you arrange follow-up testing.
Be sure to get follow-up care without delay. If breast cancer is found, it can be treated. With standard treatment, people who have breast cancers found by screening mammography have a high chance of survival.
Learn more about follow-up after an abnormal mammogram.
Susan G. Komen® Support Resources |
|
Updated 01/23/24


