Findings on a Mammogram and Mammogram Results
Mammography uses X-rays to create images of the breast. These images are called mammograms.
Learn more about mammograms.
Learn about getting a mammogram.
Mammography images
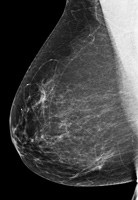
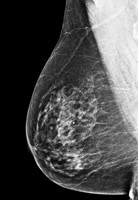
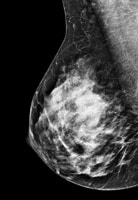
Like other X-ray images, mammograms appear in shades of black, gray and white, depending on the density of the tissue (see images below).
Very dense tissue, like bone, shows up as white on an X-ray. Fat looks dark gray on an X-ray.
Breast cancer and some benign breast conditions are denser than fat and appear a lighter shade of gray or white on a mammogram.
Dense breast tissue
Dense breast tissue can look light gray or white on a mammogram. This can make abnormal findings on a mammogram hard to see.
Younger women tend to have dense breast tissue, so their mammograms can be harder to read than the mammograms of older women.
After menopause, breast density may decrease, making mammograms easier to read.
The mammograms below show a range of breast density. Some breasts are mostly fat (fatty breasts), and some breasts are mostly breast tissue (dense breasts).
 |
 |
 |
 |
| Fatty breast | Some breast density | Dense breast | Very dense breast |
Images used with permission of the American College of Radiology (www.acr.org). |
|||
Breast density after menopause
Breast density may decrease after menopause in both women who go through natural menopause and younger women who are in menopause after surgery to remove the ovaries (oophorectomy).
For women who use menopausal hormone therapy (MHT), breast density may not decrease until they stop using MHT. MHT is also called postmenopausal hormone therapy and hormone replacement therapy (HRT).
Breast density and breast cancer risk
Women with dense breasts (as seen on a mammogram) have a somewhat higher risk of breast cancer than women with fatty breasts [26-27].
However, breast density does not appear to be related to breast cancer survival [28-30].
Learn more about breast density and breast cancer risk.
Screening tests under study for women with dense breasts
Dense breast tissue can make abnormal findings hard to see on a mammogram. Screening tools are under study for women with dense breasts.
There are no special recommendations or breast cancer screening guidelines for women with dense breasts. However, your health care provider may suggest other types of breast imaging in addition to regular mammograms.
Breast density legislation
Many states in the U.S. have laws requiring health care providers to notify (send a letter to) women found to have dense breasts on a mammogram.
In 2019, the U.S. Congress passed national breast density legislation. The Food and Drug Administration (FDA), which regulates mammography centers, is developing regulations for notification.
Although this may seem helpful, there are no special screening guidelines for women with dense breasts. However, your health care provider may suggest other breast imaging in addition to regular mammograms.
If you have any concerns about your breast density or your risk of breast cancer, talk with your health care provider.
Findings on a mammogram
Benign (not cancer) breast conditions
Some common benign breast conditions, such as cysts and fibroadenomas, may show up on mammograms as round or oval patches with distinct borders. These changes are not concerning for cancer, and these findings are not abnormal.
Learn more about benign breast conditions.
Calcifications and microcalcifications
Calcifications are bits of calcium that can show up on mammograms as small, bright white spots.
Most calcifications are benign (not cancer). However, certain patterns of calcifications are suspicious and need more testing. Tight clusters or lines of tiny calcifications (microcalcifications) can be a sign of breast cancer.
Calcifications are common, especially after age 50 [31]. They may be related to past injury to the breast or mastitis (an infection in the breast) [31].
In women treated for breast cancer in the past, calcifications may be related to past breast surgery or radiation therapy [31].
Calcifications are not related to the amount of calcium in your diet [31].
Architectural distortion
Architectural distortion describes a distorted shape or pattern of breast tissue on a mammogram. However, no mass is seen.
Although the breast tissue may be normal, this finding usually needs follow-up testing because it may be a sign of a benign (not cancer) breast condition or breast cancer.
Ductal carcinoma in situ (DCIS)
Ductal carcinoma in situ (DCIS) is a non-invasive breast cancer.
On a mammogram, DCIS usually looks like a cluster of microcalcifications. It can be hard to know from a mammogram whether the cluster is DCIS or invasive breast cancer. A cluster of microcalcifications can also be a benign (not cancer) finding on a mammogram.
Learn about follow-up after an abnormal mammogram.
Learn more about DCIS.
Invasive breast cancer
Invasive breast cancer can look like a white patch or mass on a mammogram.
The tumor cells that began in the milk duct don’t stay within the clear borders of the duct. Instead, they invade the nearby breast tissue. The outer edges of these cells look fuzzy or spiky (called spiculated).
Learn about follow-up after an abnormal mammogram.
The following is an interactive model of what a mammogram may show.
Mammography results
When to expect mammography results
Some centers give you the results of your mammogram at the time of your screening. With others, it may take up to 2 weeks to get your results.
If you don’t get your results within 2 weeks, contact your health care provider or the mammography center.
Don’t assume the results were normal because you didn’t get a report. Follow up to get your results.
Breast Imaging Reporting and Data System
Most mammography centers report the results of mammograms using the Breast Imaging Reporting and Data System (BI-RADS®).
BI-RADS® was developed by the American College of Radiology to provide a standard way to describe mammography findings (with categories numbered 0 to 6).
Updated 11/30/22

