Susan G. Komen applauds the actions taken today by the Biden-Harris Administration to bring a renewed spotlight on the Cancer Moonshot and setting an ambitious goal to reduced cancer deaths over the next 25 years by 50 percent. We believe that equitable access to affordable, high-quality care for all patient populations is essential in reducing cancer deaths and we look forward to working with the administration to remove barriers to care that contribute to cancer deaths every year.
As part of today’s announcement, the White House shared a call to action on cancer screenings, especially those missed or delayed because of the COVID-19 pandemic. The data clearly indicates that the pandemic is causing people to delay life-saving breast cancer screenings, which will lead to more advanced cancers, and an increase in mortality related to breast cancer:
- Dr. Ned Sharpless, Director of the National Cancer Institute, published analysis in Science that modeled the effect of COVID-19 on cancer screening and treatment for breast and colorectal cancer, which suggested almost 10,000 excess deaths from breast and colorectal cancer in the next decade[1]. Dr. Sharpless notes that this is almost certainly an underestimate as the model assumes only a “moderate disruption in care that completely resolves after six months,” when it is clear that the care disruptions associated with COVID-19 have been severe and have lasted much longer than six months.
- Another study estimated that the onset of the COVID-19 pandemic is associated with a decline of more than 3.9 million breast cancer screenings in 2020, compared to 2019[2].
- Other models, based on data from the three-month period from early March 2020 through early June 2020, suggest that there could be as many as 36,000 missed or delayed diagnoses of breast cancer because of COVID-19.[3]
- The CDC reviewed its data and found that in April 2020, the total number of cancer screening tests received through the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) declined by 87 percent as compared with the previous 5-year averages for that month[4].
- Additionally, the CDC highlighted a clear decline in cancer screening among women of racial and ethnic minority groups with lower incomes when their access to medical services decreased at the beginning of the pandemic. NBCCEDP has a long road ahead of not only reaching new populations that may have become eligible due to the COVID-19-related financial crisis, but also retaining those who were already eligible but delayed screening in an effort to avoid infection.
To address missed and delayed breast screenings, and ultimately have people diagnosed earlier, we know a comprehensive approach is required.
One critical aspect that must be addressed is the prioritization and investment in the NBCCEDP. Unfortunately, at current funding levels NBCCEDP serves fewer than 15 percent of the estimated number of eligible people for breast cancer screening services.
Ensuring adequate NBCCEDP funding is key to guaranteeing that low-income, uninsured and underinsured people across the country continue to have access to vital screening and diagnostic services, health education and patient navigation services, as well as enabling proper monitoring of state and local breast cancer patterns and trends. This is especially important as we work to get people back to screening, and as many Americans are experiencing job loss and financial difficulties related to the COVID-19 pandemic.
Our renewed commitment to the Cancer Moonshot and bringing people back to cancer screenings must be paired with a robust investment in programs such as NBCCEDP, which have a proven track record.
In coordination with today’s announcement the White House released a report, Closing Gaps in Cancer Screening, which states that, “Cancer screening saves lives; however, gaps in screening uptake and timely receipt of follow-up care after an abnormal screening test result mean too many people are unnecessarily enduring aggressive treatment or dying from cancers that could have been prevented or detected at earlier stages.”
We have heard far too often from the breast cancer community about the financial barriers to needed follow-up diagnostic imaging that limit their ability to remain in the screening continuum – an additional issue that must be addressed in a comprehensive approach to earlier detection of breast cancer.
Studies show that individuals facing high out-of-pocket costs associated with diagnostic imaging are less likely to receive that follow-up imaging. This can mean that the person will not seek care until the cancer has spread to other parts of the body making it much deadlier and much more costly to treat.
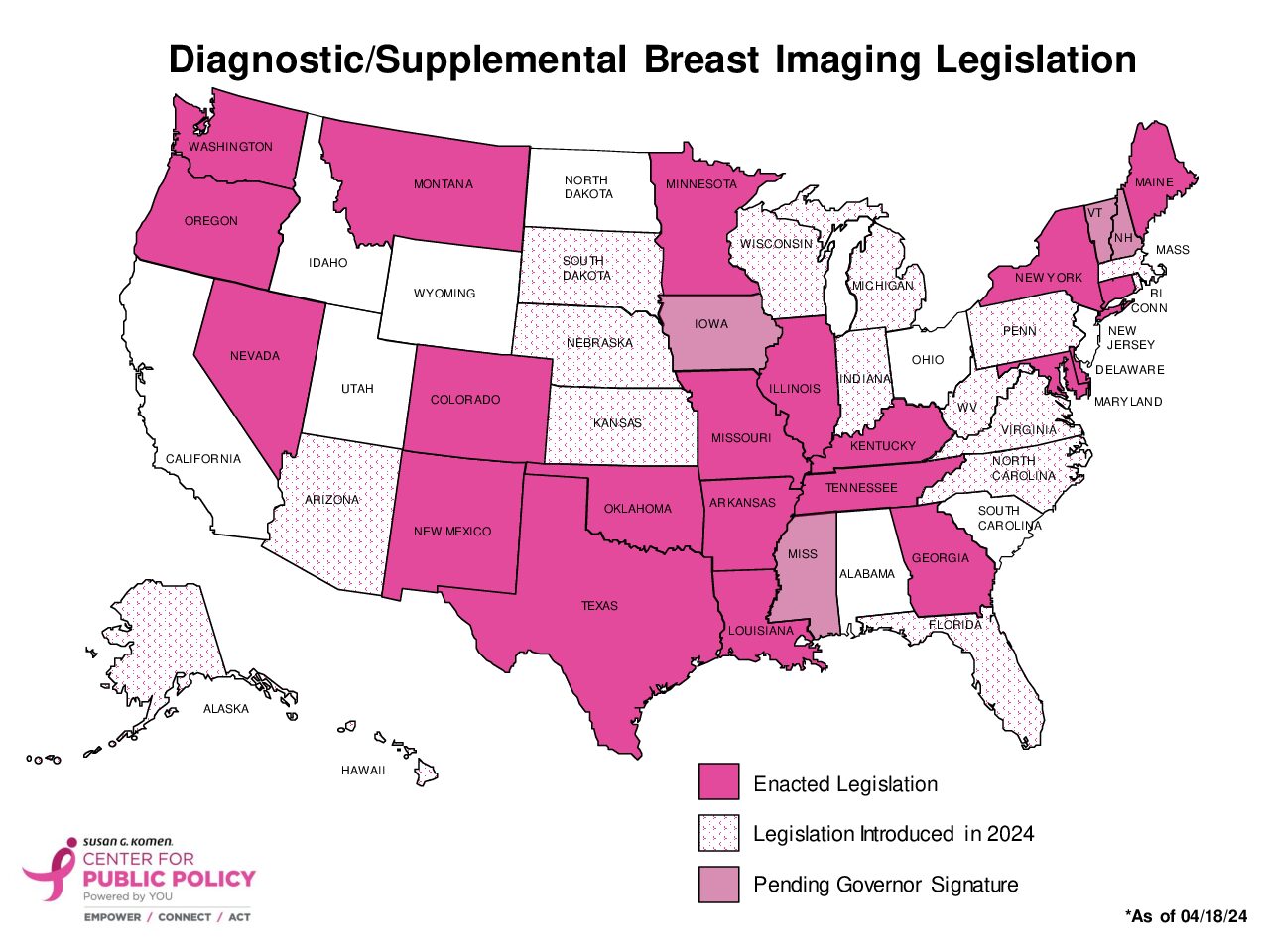
Komen’s Center for Public Policy has been leading efforts in state legislatures across the country and at the federal level in Washington, D.C. to pass legislation that eliminates patient out-of-pocket costs for required diagnostic imaging. To date, this issue has been addressed in six states (Arkansas, Colorado, Illinois, Louisiana, New York, and Texas) with more than 10 states introducing legislation in 2022. The Access to Breast Cancer Diagnosis Act has been reintroduced in the U.S. House and Senate and is pending action in both chambers.
Komen shares the goal of the administration “to detect cancers when there may be more effective treatment options,” but we need support now from policymakers to make this goal a reality for all by expanding access to screening and diagnostic imaging services while also reducing the burden that falls on the shoulders of patients.
Join in on our efforts advocating for these needed changes and others.
Molly Guthrie is Susan G. Komen’s Sr. Director of Public Policy and Advocacy.
[1] Sharpless, Norman E. COVID-19 and Cancer. Science. 19 JUNE 2020 , VOL 368 ISSUE 6497. DOI: 10.1126/science.abd3377
[2] Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of Cancer Screening Deficit in the United States With the COVID-19 Pandemic. JAMA Oncol. 2021;7(6):878–884. doi:10.1001/jamaoncol.2021.0884
[3] IQVIA Institute for Human Data Science, Shifts in Healthcare Demand, Delivery and Care During the COVID-19 Era (April 2020)
[4] A. DeGroff, J. Miller, K. Sharma, et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January–June 2020, in the United States. Preventive Medicine, Volume 151, 2021, 106559, ISSN 0091-7435, https://doi.org/10.1016/j.ypmed.2021.106559.